< View all

<
The Smartest People In The Room®
Market access strategy for a regional provider network
Market access strategy for a regional provider network
Redesigned the market access strategy for a multi-hospital network, expanding patient reach and increasing commercially-insured specialty volumes by 27% within the first year. Showed that “market access” is not just a marketing function; it’s a system-level growth lever that unites clinical capacity, digital visibility, and referral alignment to capture patients who were already in the market but couldn’t find or reach the system.
2
min.
read

Issue/opportunity
A $2.5B regional health system was losing patients to competitors despite strong clinical programs. Access constraints (long appointment lead times, limited evening/weekend availability), disjointed scheduling platforms, and low digital visibility led to leakage of high-margin cardiology and oncology patients. The system lacked a cohesive view of where patients originated, where they left, and why.
Approach & outcomes
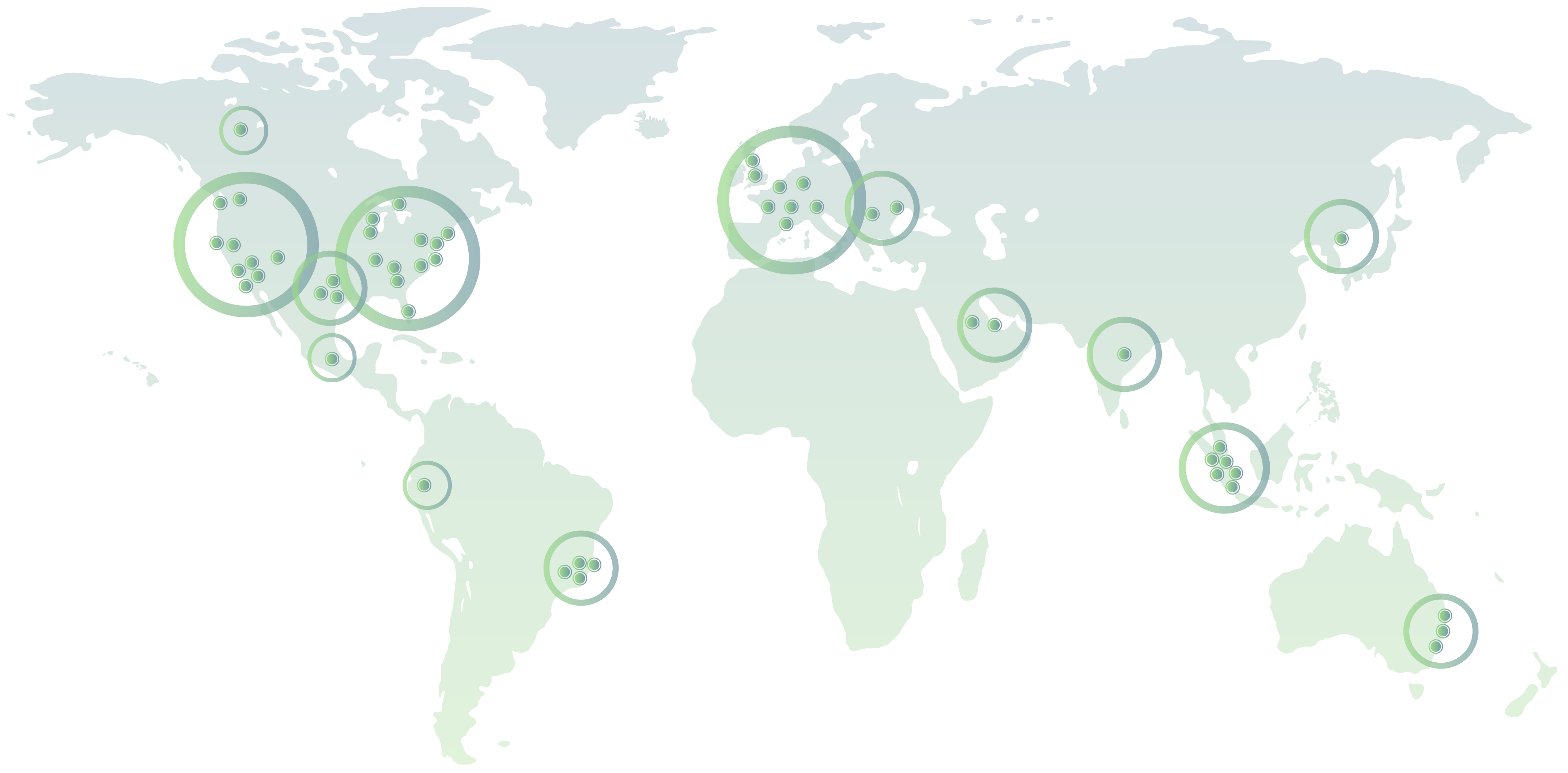
- Geospatial Access Mapping: Combined claims, EHR, and census data to identify high-demand zip codes with low in-system penetration.
- Access Expansion Model: Designed a hub-and-spoke coverage plan that added urgent access clinics and co-located specialists within PCP offices.
- Scheduling & Referral Redesign: Implemented centralized scheduling, digital self-service booking, and referral routing to the nearest in-network specialty site.
- Digital Front Door Activation: Enhanced online presence, search optimization, and targeted outreach to commercially-insured populations.
- Payer & Employer Alignment: Partnered with top regional payers and employer groups to steer members toward new access points.
Results
- 27% increase in commercially-insured specialty visits.
- 14% reduction in appointment wait times across high-volume specialties.
- 19% decrease in out-of-network leakage within six months of launch.
- Achieved full ROI within nine months through increased downstream revenue and payer incentives.
Meet the Author


No items found.